The Six Links in the Chain of Transmission &
Breaking the Chain of Transmission
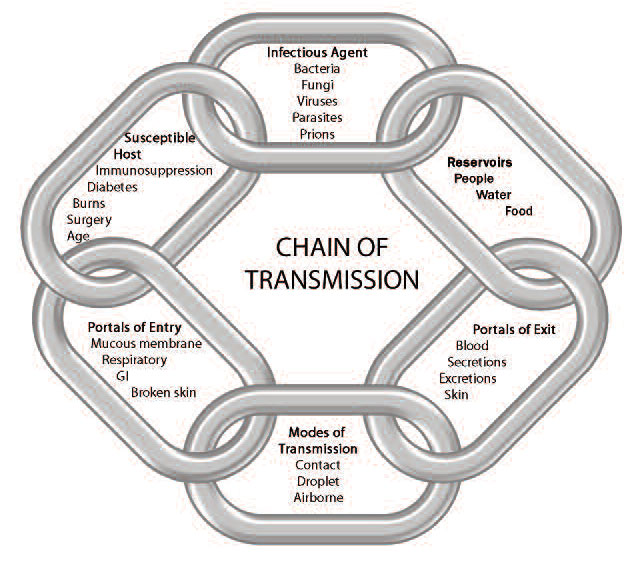
Chain Of Transmission
Each link in the chain represents a factor related to the spread of microorganisms. Transmission of infectious agents does not take place unless all six of the elements in the chain of transmission are present. Public Health of Ontario
©Queen’s Printer for Ontario, 2011. Adapted with the permission of Public Health Ontario.
Did You Know?
Public Health Ontario has a set of free infection prevention and control learning modules.
Infection Prevention and Control – Online Learning | Public Health Ontario
The links in the Chain of Transmission can be broken through a careful Risk Assessment and consistent application of Routine and Additional Precautions, where indicated.
| Links in the Chain of Transmission are: | Breaking the Chain of Transmission by Assessing: |
|
|---|---|---|
| INFECTIOUS AGENT | The micro-organisms capable of producing infection (e.g., bacteria, viruses) | The pathogenicity/virulence of the infectious agent |
| RESERVOIR | The places in which the infectious agent lives (e.g., humans, animals, water) | The patient/client’s environment (e.g., shared facilities, such as multi-bed rooms) |
| PORTAL OF EXIT | The point where the agent leaves the reservoir (e.g., blood, secretions) | The potential for exposure to blood, body fluids, secretions and excretions (e.g. splashing, patient coughing) considering the duration of exposure (e.g., sterile gown for central line insertions) |
| MODES OF TRANSMISSION | Contact – which is divided into: • Direct Contact – occurs through touch • Indirect Contact – occurs when micro-organisms are transferred by contaminated object coming into contact with another surface | the procedure(s)to be performed (e.g., hand hygiene & PPE required) and whether Additional Precautions are required • whether there will be contact with non-intact skin or mucous membranes • the potential for handling sharp or contaminated instruments or equipment |
| Droplet Transmission – occurs when large droplets exit the respiratory tract of a person when they cough or sneeze. Can also be generated by some procedures (e.g., suctioning). These droplets are projected at a short distance of usually < 2m and enter the hosts eyes, nose, mouth or fall onto surfaces. | ||
| Airborne Transmission – occurs when airborne particles remain suspended in the air, travel on air currents and are then inhaled by others who are nearby or who may be some distance away from the source patient, in a different room or ward (depending on air currents) or in the same room that a patient has left, if there have been insufficient air exchanges. |
||
| Parenteral Transmission – the spread of an agent through intact skin by a sharp (e.g., needle stick injury). | ||
| Common Vehicle Transmission – the spread of an agent through a common contaminated source (e.g., multi-dose vials) | ||
| Vector Transmission – occurs when a host is bitten by an animal or insect carrying the infectious agent (e.g., mosquito transmitting West Nile virus) | ||
| PORTAL OF ENTRY | The point at which the agent enters the host (e.g., non-intact skin, respiratory or GI tract, mucous membranes) | The need for aseptic technique for invasive procedures and handling injectable products. The appropriate catheter and wound care |
| SUSCEPTIBLE HOST | Any person at risk of infection (e.g., immunosuppressed patients, burn victims, elderly) | The need for appropriate immunization |
References
Association for the Advancement of Medical Instrumentation (AAMI). (2015). FDA proposes new criteria for surgical gowns. Retrieved from Association for the Advancement of Medical Instrumentation website: www.aami.org/newsviews/newsdetail.aspx?ItemNumber=2650
Canadian Patient Safety Institute. (n.d.). Ventilator-associated pneumonia (VAP). Retrieved from Canadian Patient Safety Institute website: www.patientsafetyinstitute.ca/en/topic/pages/ventilator-associatedpneumonia-(vap).aspx
Centers for Disease Control and Prevention. (2011). Central line-associated bloodstream infections: Resources for patients and healthcare providers. Retrieved from Centers for Disease Control and Prevention website: www.cdc.gov/HAI/bsi/CLABSI-resources.html
Critical Care Secretariat. (2012). Ventilator associated pneumonia and central line infection prevention toolkit. Retrieved from Critical Care Services Ontario website: www.criticalcareontario.ca/EN/Toolbox/Performance%20Improvement%20Collaborative/VAP%20and%2 0CLI%20Toolkit%20(2012).pdf
Immunize Canada. (2016). ImmunizeCA app. Retrieved from Immunize Canada website: http://immunize.ca/en/app.aspx
Loeb, M., Dafoe, N., Mahony J., John, M., Sarabia, A., Glavin, V., Walter, S.S. (2009). Surgical mask vs N95 respirator for preventing influenza among health care workers: A randomized trial. JAMA, 302(17), 1865- 1871. doi:10.1001/jama.2009.1466. Retrieved from http://jama.jamanetwork.com/article.aspx?articleid=184819
PIDAC. (2012a). Best practices for infection prevention and control programs in Ontario (3rd ed.). Retrieved from Public Health Ontario website: www.publichealthontario.ca/en/eRepository/BP_IPAC_Ontario_HCSettings_2012.pdf
PIDAC. (2012b). Routine practices and additional precautions in all health care settings (3rd ed.). Retrieved from Public Health Ontario website: www.publichealthontario.ca/en/eRepository/RPAP_All_HealthCare_Settings_Eng2012.pdf
PIDAC. (2013). Annex B: Best practices for prevention of transmission of acute respiratory infection in all health care settings. Retrieved from Public Health Ontario website: www.publichealthontario.ca/en/eRepository/PIDAC-IPC_Annex_B_Prevention_Transmission_ARI_2013.pdf
PIDAC. (2014). Best practices for hand hygiene in all health care settings, (4th ed.). Retrieved from Public Health Ontario website: www.publichealthontario.ca/en/eRepository/2010-12%20BP%20Hand%20Hygiene.pdf
PIDAC. (2015a). Best practices for prevention, surveillance and infection control management of novel respiratory infections in all health care settings. Retrieved from Public Health Ontariowebsite: www.publichealthontario.ca/en/eRepository/Best_Practices_Novel_Respiratory_Infections.pdf
PIDAC. (2015b). Infection prevention and control for clinical office practice. Retrieved from Public Health Ontario website: www.publichealthontario.ca/en/eRepository/IPAC_Clinical_Office_Practice_2013.pdf
PIDAC. (2016). Tools for preparedness: Triage, screening and patient management for Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infections in acute care settings. Retrieved from Public Health Ontario website: www.publichealthontario.ca/en/eRepository/PIDAC-IPC_Preparedness_Tools_MERS_CoV_2013.pdf
Public Health Agency of Canada. (2013). Canadian immunization guide. Retrieved from Public Health Agency of Canada website: http://phac-aspc.gc.ca/publicat/cig-gci/p03-work-travail-eng.php#a1
Public Health Agency of Canada. (2014). Canadian Tuberculosis Standards (7th ed.). Retrieved from http://www.phac-aspc.gc.ca/tbpc-latb/pubs/tb-canada-7/assets/pdf/tb-standards-tb-normes-prefeng.pdf
Public Health Agency of Canada. (2016). Summary of assessment of public health risk to Canada associated with Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Retrieved from Public Health Agency of Canada website: www.phac-aspc.gc.ca/eri-ire/coronavirus/risk_assessment-evaluation_risque-eng.php
Public Health Ontario. (n.d.a). Chain of transmission and risk assessment: Glossary of terms. Retrieved from Public Health Ontario website: www.publichealthontario.ca/en/LearningAndDevelopment/OnlineLearning/InfectiousDiseases/IPACCore/Documents/CORE_Trainers_COT_and_RA_Module_Glossary_April _2014.pdf
Public Health Ontario. (n.d.b). Risk Algorithm to Guide PPE Use. Retrieved from Public Health Ontario website: www.publichealthontario.ca/en/eRepository/IPAC_Clinical_Office_Practice_Risk_Algorithm_PPE_2013.pdf
World Health Organization. (2015). Middle East respiratory syndrome coronavirus (MERS-CoV). Retrieved from World Health Organization website: www.who.int/mediacentre/factsheets/mers-cov/en/
